Whether you’re returning to the office, or you will continue to work from home for the foreseeable future, one thing is universal: Caring for ourselves helps us serve our clients and families and keeps us healthy.
Working from home has been a transition for many of you. You’ve had to deal with ergonomic issues that may not have seemed significant if you were only working from home a few hours a month but are very significant when you’re working from home nine or ten hours per day. When we work in isolation, we often find ourselves sitting for longer periods. We forget to move and take stretch breaks. With gyms and yoga studios closed you may be feeling stiff or sluggish.
5 Best Practices to Consider When Evaluating Your Ability to Care for Yourself and Your Clients
1. Learn How to Relax. One method to consider is the Practice of Mindfulness
What Is Mindfulness? Mindfulness is a state of intentional, nonjudgmental focus on the present moment. Mindfulness techniques are often incorporated into other practices, such as yoga or meditation. It is often thought to include the following elements:
-
- Awareness – Being tuned in to what is happening in the present moment, including sights, sounds, smells, or physical sensations you might usually ignore.
- Focus – Paying attention to the present moment, without thinking about past or future events.
- Acceptance – Accepting whatever you might be feeling or thinking, without judging it or trying to change it or your reactions.
- Observation – Recognizing unpleasant sensations, thoughts, and feelings as temporary and fleeting, observing them objectively without reaction or judgment.
What Are the Benefits of Mindfulness? Mindfulness has been studied for many years. According to recent research, it has several benefits for physical and mental health. Some of the strongest health benefits include:
-
- Improves mood – Mindfulness training may reduce depression and anxiety. One study found that mindfulness training was as effective as antidepressant medications in preventing a depression relapse.
- Reduces stress and its consequences – Mindfulness can lead to less intense stress responses. This has many health benefits, such as lowering your blood pressure and strengthening your immune system.
- Improves coping with pain –People with chronic pain who practice mindfulness meditation report less severe pain and pain-related distress. They are also more active despite their pain.
- Improves brain functions – Practicing mindfulness helps build your ability to pay attention and focus. Over time, this training can sharpen memory and improve mental performance.
- Helps with weight management – Some mindfulness techniques have been shown to reduce overeating and obesity.
2. Connect with a Support System
Don’t forget to continue to connect with your worksite and your friends. It is worth the effort! Your employer may have an Employee Health Department, an EAP provider or a Human Resources representative. They are there to help you come up with an effective plan for managing your stressors, so you can perform your best on the job.
Your friends can also be a wonderful support system but also keep you accountable if you choose to begin a program to increase your fitness level. Grab a buddy and get out there! You are more likely to keep that commitment as you won’t want to let the team down.
3. Keep A Stress or Gratitude Journal
Writing down items or thoughts that stress you, or perhaps even items that upon reflection you are grateful for can be cathartic. It allows you to self-reflect, can help you to keep your thoughts organized, and help you to deal with your big thoughts in a healthy and safe way. On a positive note, as you record your ideas on-the-go, you can improve your writing skills.
4. Take your Vacation Time and Reboot
I am sure you are finding yourself working at all hours of the day, during this “Stay at Home, Work Safe” timeframe. It is much harder to switch off when your office is in your home.
We at CompAlliance are encouraging our staff to set up a “staycation” with their families. Just because we cannot travel at this time, doesn’t mean we should not take a break from work. Employees who take time off from work report feeling less stress, less anxiety, and fewer instances of depression. Those aren’t the only positive effects, either; regular vacations are linked to lower risk for heart disease, and the experience of a vacation is shown to have a lasting impact on general wellbeing and a perception of a life well-lived.
Happier, healthier employees are more productive. We Americans tend to leave vacation time on the table every year. Final note on this, don’t check in on work while you are on staycation.
5. Break away from media
In today’s digital world, it’s easy to feel pressure to be available 24 hours a day, especially when you have been working from home. If you find yourself spending significant time reading email, social networking sites, watching media coverage of the pandemic and notice this is increasing your stress level, consider setting up structured amounts of time on these activities. Use trusted sources for your pandemic news, e.g., the CDC.
CompAlliance is proud to also offer our clients additional resources to maintain your health and well-being.
CompAlliance has partnered with Restore and Renew to bring you a series of free, twice-weekly yoga virtual classes.
These classes vary in length from 10-minute, quick breaks that can be done from your chair, to 30-minute sessions you can enjoy during your lunch hour or even before or after work. Each class is offered with instruction suitable for beginners or the seasoned yoga practitioner. You’ll walk away feeling relaxed, refreshed, and with renewed energy levels. You’ll be ready to serve your clients and maintain your health and vibrance. Click here to register for these sessions.
CompAlliance Resources to Maintain Your Health and Well-being and Assist Your Recovering Workers. Following are links to some of these resources.
Blog article – Getting Ready for Work as the Pandemic Levels Our or (Get Up Offa That Thing)
Virtual Ergonomic Training – Keeping Your Newly “Stay Home, Work Safe” Employees’ Worksite Safe
24/7 Telephonic Coronavirus (COVID-19) Nurse Triage – Helping to clarify and offer alternatives
Hypothetical Employability Evaluation – Assisting in determining the potential for a Recovering Worker’s Capabilities to Return to Work
Alternative Transitional Duty – Yes even during these trying times your Recovering Worker can be placed in an essential volunteer position to assist with transitional Return to Work
CompAlliance is honored to be your Managed Care Services Provider during these trying times.
Evaluating Self-Care and Care for Others Printer-Friendly Page
It is important to determine whether your case management software system can meet the needs of your staff and your referral source.
- Can it keep track of your case manager’s notes and daily activities?
- Will my case management software produce an invoice that accurately reflects both the activity on the file and in keeping with my client’s Special Handling Instructions?
- Can I generate progress reports for the referral source?
- Does it keep an accurate case log of my case manager’s activity?
- Can I link medical reports to the case?
After the case management software system validates these basic requirements you may want to consider the following best practices to assist in choosing the system that best meets your needs.
5 Best Practices to Consider When Evaluating Case Management Software
- Is the software easy to use while still collecting the data you need? Software applications can create incredible efficiencies and provide invaluable data to your customer – if they are easy to use. Decision makers want data, but if your users have a difficult time entering data because it requires them to navigate a maze of menu items, your productivity will decrease at the expense of data collecting.
The gold standard for case management systems include user interfaces geared towards case manager productivity, while collecting and storing valuable data for future use. Additionally, a system should ensure minimizing workflow adjustments to end users when new features are made available. It is essential to ensure optimal workflow efficiencies while not trading off valuable data assets.
- Does the software change the way you work? Is it a positive or negative change? We all know that change can be scary, especially if you have been trained to do things a certain way. “If it’s not broke, then why fix it” is a question frequently asked by the staff when being asked to make this change.
For example, the billing life cycle can be a pain point particularly when you work with several service lines, across multiple regions, with specific billing exceptions, rules, and handling instructions unique to each client. This can be a great candidate for process improvement. The case management system can make noting these exceptions superfluous to the user, as they can be input once and then accurately utilized by the entire team. The case manager is then only concerned with providing timely, quality case management services.
This would be a change even your most resistant staff could embrace. Ask the software vendor to run through some of your most common case management workflows and see for yourself if the solution gives time back to your case managers.
- Will the vendor be able to support my case managers? In addition to ensuring the case management software you are evaluating meets your functional requirements, make sure the vendor has a structured end-user support system in place. This will prevent frustrated case managers unable to perform their work because they forgot how to perform a task or something is simply not working.
To assess for this end-user support, assess what type of support is offered post implementation? Is there phone/email support? What are their live support hours? What are your SLAs (service level agreements)? Are there manuals, reference guides or knowledge bases available? Although some may argue that an intuitive case management system should be self-explanatory, manuals and reference guides serve as a sort of safety blanket for the end-user. Users inherently want to use a system correctly, and reference manuals are the de-facto way vendors communicate the “preferred” way of using their software.
- Does the case management software use a modern infrastructure? Is the software hosted on the cloud? There are several advantages that are realized by having your case management software hosted on a cloud infrastructure. Scalability, availability, disaster recovery, and performance are a few of the most important. If the case management software is not hosted in a cloud type environment you will need to understand the rationale, though current best practices are use of a cloud environment.
- Security, Security, Security– Did we mention security? It doesn’t matter if the case management software you are evaluating checks off all the items discussed above and more, if the platform is not secure or if the vendor does not have a proven track record for security. A vendor that minimizes or does not stress the importance of security, leaves your entire operation exposed to potential data breaches. Current best practice is to require SOC2 compliance.
In conclusion, do your own extensive risk assessment prior to selecting your case management software vendor. Ask the vendor to provide their policies regarding IT governance, change management, and access management. It will be hard and time consuming, but this exercise will help to mitigate disastrous consequences in the future.
Introduction to your Employee’s Alternative Transitional Duty Program
When an employee experiences injury, illness, or disability that causes him or her to lose time from work, he or she will likely interact with, at a minimum, medical practitioners and claims administrators. These professionals have their own specialized responsibilities and goals, which aren’t necessarily aligned with the Stay at Work/Return to Work (SAW/RTW) interest of either the employer or the employee. For example, medical practitioners tend to focus on diagnosis and treatment, not on functional and RTW outcomes, which have not traditionally been within the purview of medicine. They are typically not trained in the benefits of RTW and may not consider the options that accommodations could provide a worker or have a full understanding of tasks specific to a given job.
The employer may be more concerned about how best to get the work done in the employee’s absence than with the worker returning to work. Likewise, the claims administrator may have a large caseload and cannot focus the time needed to facilitate transitional SAW/RTW opportunities either with the employer or in an alternate setting.
The goal of an ATD program is to facilitate recovering workers remaining at or returning to work as soon as medically appropriate, following an injury. A timely SAW/RTW can make a significant impact on lowering the cost of a workplace injury. If the employer of injury is unable to accommodate a light duty program at their facility, an ATD program may be the answer to getting some of these costs under control. Statistics show that the longer a recovering worker remains off work, the more probable it is that they may never return. There is only a 50% chance an injured employee will RTW after a six-month absence, and this declines to a 25% chance following a one-year absence.
Five Best Practices to Look for When Considering an ATD Vendor
- Make sure your staff providing transitional duty services are credentialed, possess a graduate degree and are licensed in some type of clinical profession, such as counseling. A certified and licensed rehabilitation professional has the experience and education to effectively intervene and address concerns voiced by the recovering worker as we work towards a transitional SAW/RTW. A rehabilitation professional has the experience to ensure the transitional job is appropriate to the functional requirements.
If the appropriateness of the position is contested or litigated by the injured worker and their representative, you want an expert in the field of rehabilitation able to testify as to the appropriateness of the position. A rehabilitation professional also has the expertise to document objectively regarding any barriers or observed sabotage on the part of the recovering worker. Some of the recommended credentials include:
-
- Master’s degree in Rehabilitation, Education or Psych
- Certification as a Rehabilitation Counselor
- Certified Ergonomic Assessment Specialist
- Some type of clinical licensure
- Use a company with experience in placing employees from a workers’ compensation case management perspective. Having knowledge of how to manage the ongoing needs of the injured worker and their employer as they progress through a transitional duty program is invaluable.
- FOLLOW UP with the employer and the injured worker on an ongoing basis is essential. The rehabilitation professional can explore any objections and work with all parties to come up with a mutually agreeable and beneficial plan. Assessing and documenting attendance and ensuring timely communication of same to ensure payroll can be processed promptly.
- Prepare and collaborate with the injured worker to facilitate their connection to the mission of the volunteer organization. Work with the injured worker to ensure their proper workplace skills, e.g., prompt and consistent attendance, to schedule therapy sessions if needed outside of the work schedule, etc. Ensure your vendor has a system in place to ensure proper initial and ongoing documentation including reports, letters, timecards, attendance emails, etc.
- Your vendor should have an established database of non-profit organizations nationwide they have worked with.
In conclusion, the success of your Alternative Transitional Duty Program depends on setting up Best Practices to ensure a consistent and collaborative approach to a SAW/RTW program that gets your employee back to work as soon as medically appropriate!
Evaluating Alternative Transitional Duty Printer-Friendly Page
When the Recovering Worker is Unable to Return to the Job of Injury with the Employer
Even with the finest medical case management, on occasion a recovering worker’s post injury functional capabilities will prevent a return to their job of injury with the employer. When a return to work at the pre-injury level is not an achievable goal, a nationally certified Vocational Expert can work with the recovering worker towards the goal of returning the individual to employment consistent with their functional capabilities and skills.
Five Best Practices to Look for When Considering a Vocational Case Management Vendor
- Does the Vocational Consultant perform an initial assessment? Look for a comprehensive:
- Vocational work history
- Education history
- Hobbies and interests
- Medical status and RTW capabilities
- Psychosocial – motivation for RTW, family history and support
- Assessment of barriers to RTW
- Make sure your staff providing Vocational Rehabilitation services are credentialed, possess a graduate degree and are licensed in some type of clinical profession, such as counseling. A certified and licensed rehabilitation professional has the experience and education to effectively intervene and address concerns voiced by the recovering worker as we work towards a transitional SAW/RTW. A rehabilitation professional has the experience to ensure the transitional job is appropriate to the functional requirements.
If the appropriateness of the vocational assessment, positions found or findings are contested or litigated by the injured worker and their representative, you want an expert in the field of rehabilitation able to testify as to the appropriateness. A rehabilitation professional also has the expertise to document objectively regarding any barriers or observed sabotage on the part of the recovering worker. Some of the recommended credentials include:
-
- Master’s degree in Rehabilitation, Education or Psych
- Certification as a Rehabilitation Counselor
- Certified Ergonomic Assessment Specialist
- Some type of clinical licensure
- Use a company who advocates for weekly contact with the recovering worker, ensures the recovering worker knows they are accountable for their own results, and assists the recovering worker to take ownership of their own vocational rehabilitation process. Does your vendor provide Job Seeking Skills Training for the recovering worker? Ask if during their weekly meetings with the recovering worker, are they open and discuss their opinion of the recovering worker’s status and provide encouragement, suggestions, etc. to facilitate success whenever possible?
- Communication Skills are essential. Does your vendor provide training for their internal staff in topics such as Motivational Interviewing, Cultural Diversity, and Ethical Decision Making? Ask to see their training records. Do they provide financial support for ongoing training for their staff, to facilitate earning the CEUs required to retain certification?
This type of ongoing training provides the skills the vocational staff need when meeting with the recovering worker to develop a collaborative written rehab plan, to explore any objections, and work effectively with all parties. It is essential they seek and obtain agreement from the recovering worker and their legal representative, if they have one, regarding this plan.
- Discuss with your vendor their process for obtaining and providing documentation and follow up – with employers, the recovering worker and their legal representative. Do they verify data provided by the recovering worker during the job search phase? How often do they follow up? What does the documentation look like? Will it be helpful if litigation ultimately ensues? What is their process for working with the recovering worker when noting issues? What type of reporting do they provide? Will they modify their standard reporting to meet your specific requirements?
In conclusion, the success of your vocational services program depends on a variety of factors including the education level of the staff providing the services, the support from their company to continue participation in continuing education, their understanding of the need for collaboration with the recovering worker and the type and frequency of documentation during the process.
Evaluating Vocational Case Management Services Printer-Friendly Page
When Should You Use the Services of a Field-based Case Manager?
Field-Based Case Management is the process of utilizing a Medical Case Manager to assist the claims professional with assuring appropriate, goal-directed, timely medical treatment and facilitating a consistent, progressive return to work program with the goal of an appropriate and timely resolution of the claim. In many cases, Medical Case Management can be utilized through the services of either an in-house or externally hired Telephonic Case Manager. However there are certain circumstances when it may be most appropriate to utilize the services of a field-based case manager.
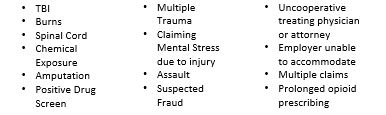
Examples of appropriate Field-Based Case Management Assignments:
Five Best Practices to Look for When Using the Services of a Field-Based Medical Case Manager
- Are your Case Managers proactive or reactive? Case Managers must approach every interaction with the recovering worker and the physician with a proactive frame of mind. They have to think what question can I ask at today’s exam to move this case in the direction toward recovery and return to work? They also need to ask how will I respond if the recovering worker or provider asks questions of me? This takes preparation and planning prior to each medical exam.
- Thorough and prompt communication. It is imperative that Case Managers be the primary spoke in the wheel of communication among all parties involved in a workers’ compensation claim. The communication needs to take place within one business day of all significant changes and appointment updates, as well as to discuss with Recovering Workers any possible questions or concerns they may have regarding the plan of care.
- Does your Case Manager understand their role? It is important for your Case Manager to acknowledge their role as a facilitator of medical treatment, to coordinate care, act as an educator and advocate for the recovering worker and to ensure communication between all stakeholders. It is equally as important for Case Managers to know what falls outside of the CM role, and to defer all legal, employment, and benefit questions to the appropriate specialists in those areas; the claims professional, the defense or respondent attorney, and employer.
- Can your Case Manager Adapt? Case managers must be adaptive to multiple practice settings in which the recovering workers receive not only health care and services, but be able to identify and access related human services that may be needed to ensure success and progression. Success comes with the ability to look at the entire situation and services that are available.
- What evidence based medicine guidelines does your case management company utilize? Use of evidence based guidelines is essential when collaborating with the treating physician, determining if they are practicing within accepted treatment guidelines, and having an objective database to utilize when discussing any discrepancies. This information is also beneficial for use when sharing with the recovering worker the anticipated treatment and recovery plan.
In conclusion, these Best Practices are the ingredients needed for quality outcomes of your work-related injuries with the goal of a timely and medically appropriate return to work for your Recovering Worker.
Evaluating Medical Case Management Service Printer-Friendly Page
Utilization Management / Utilization Review (UM/UR) is an Effective Tool to Assure the Recovering Worker Receives the Most Appropriate Treatment, with a Goal of Return to Health and Function.
CompAlliance believes there is a difference between a proactive Utilization Management approach and a reactive Utilization Review approach when facilitating appropriate care. We believe when collaborating with providers you reduce the overall claims cost, by expediting the most appropriate treatment in order to facilitate recovery and Return to Work. Conversely, when a Utilization Review program is focused on denials, they often ADD to the cost of a claim by delaying recovery and adding friction to the claim.
5 Best Practices to Look for When Using a UM/UR Provider
- Is your UM/UR Provider Outcomes-Driven? If you request your vendor produce cost-savings and ROI data, you are creating a perverse incentive to deny care that may be necessary and appropriate for recovery. “Savings” on the medical side of the claim may drive up indemnity costs. Consider taking a holistic approach to Utilization Management instead. What treatment is necessary to expedite recovery and return to work? The charts below represent two Utilization Management clients. Both illustrate the outcomes-based approach to Utilization Management drives down claim costs and speeds return to work and MMI.
- Learn from your Data. Your UM vendor should be able to provide you with extensive data about your medical providers. Use that data and claims data to refine your MPN, to create prior-authorization protocols, and expedite appropriate medical care. Some of the questions to ask while evaluating this data:
- Which providers are adhering to guidelines and have the highest approval ratings?
- Which providers are cooperating with your return to work efforts? Returning recovering employees to work with the lowest number of lost days?
- Which providers submit requests with reports that clearly support the need for treatment, versus those that require additional information to be submitted (which leads to delays and additional UM efforts)?
- What categories of treatment are always approved?
- What categories of treatment are problematic?
- Where is unnecessary friction being created?
- Get to Yes, Quickly. Does your utilization management team understand the need to approve appropriate care as quickly as possible? Expediting appropriate care facilitates recovery and return to work and is much more cost-effective in the long run than delaying care through denials on technicalities or overly strict adherence to guidelines. Guidelines are developed on a bell-curve and not every recovering worker fits in that bell-curve. If there are compelling reasons to approve outside of guidelines, your UM vendor should do so.
If you have trusted medical providers who achieve good outcomes and have good diagnostic skills, and the recovering worker meets criteria for surgery, do you really need to make them have every confirmatory diagnostic test before you approve surgery to address the underlying issue? How much cost and delay does requiring scheduling of an MRI and getting the subsequent diagnostic confirmation add to each surgical request? Is your recovering worker losing time during this additional testing timeframe?
- Use Automation, Wisely. Automation of repetitive tasks, and automation to assure timeliness, are wonderful things. Automatically matching guidelines to a given request is also very efficient, but automating clinical decisions is not as easy as it sounds. If you are trying to achieve the most expedient recovery and return to work, automatically approving treatment has its pitfalls.
At many points in the recovery process, guidelines may support any number of treatment modalities, but it still takes clinical judgement to know which is the best course of treatment, at this TIME, for this RECOVERING WORKER, with these CO-MORBIDITIES. A Utilization Management program takes an approach which says, “what is the BEST course of treatment?” First Level UM case managers are not able to deny treatment that is supported by guidelines, but the case manager can ask “could we try this…?” Most often, as reflected by the charts above, with great results.
- Know When to Say No. However, there are times when a denial of treatment is necessary. Co-morbidities may create a risk for the recovering worker, despite the fact they meet the clinical criteria for care. A diabetic with hypertension, may have meet criteria for a surgical repair of their shoulder, but are they fit for surgery? Drug interactions may pose harm to recovering workers when medications are taken together, or with certain supplements. In these cases, a denial should clearly delineate the risks to the recovering worker.
Not everyone is a good actor. We have seen the spinal hardware and toxicology schemes, the opioid crises, the compounding and topical medications that are inappropriately prescribed. These and other schemes create waste in the system, and further victimize the recovering worker in their worst forms.
In conclusion, when your UM/UR Vendor facilitates appropriate, timely care or puts a stop to inappropriate care, they are protecting the recovering worker, and ultimately that is the goal of good Utilization Management.
Evaluating Utilization Management / Utilization Review Services Printer-Friendly Page