Senators John Boozman (R-AR) and Tom Cotton (R-AR) have introduced a Senate resolution (S.Res.261) designating the week of Oct. 11–17, 2015 to honor case management professionals for their contributions to health care. This year’s theme is Case Management: A Patient’s Partner in Healthcare. This week we at CompAlliance hope to share a few thoughts on the profession of case management and the role it plays in the workers’ compensation arena.
The goal of case management is to maintain optimal patient health status across the continuum of care in a manner that emphasizes both individual control over decisions and stewardship of resources. Many states have legislated methods for choosing the providers of health care for the injured worker, however the case manager plays an important role in ensuring the injured worker understands their current health status, what they can do and why their treatment plan is important to their rehabilitation. CompAlliance believes the case manager is the catalyst for education of and collaborative communication with the injured worker, thereby facilitating an improved adherence to the treatment plan.
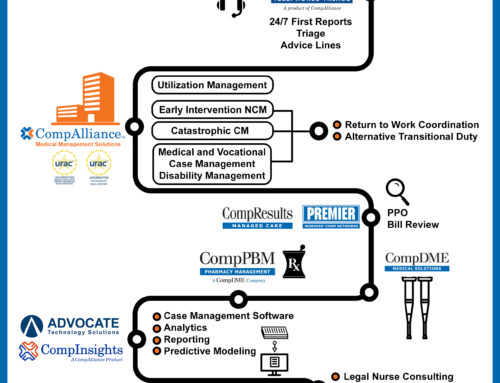
Core functions of a case manager include assessment, care coordination, patient education, monitoring of the treatment plan and status, planning for discharge from treatment, resource management and advocacy for appropriate, goal-directed treatment for the injured worker.
The case manager provides the glue for the health care team, the employer and the claims professionals and coordinates and implements a plan of care that is in keeping with the best interests of the injured worker and is at the same time goal-directed towards a medically appropriate and timely return to work.
Case management has been proven to enhance performance in areas such as clinical outcomes, patient satisfaction, resource utilization and cost-effectiveness.