Article prepared by: Glenda Garrard, Jay Garrard and Linda Van Dillen.
SB1160 addressed a wide-ranging array of issues in Workers’ Compensation, and was signed in 2016 by California Governor Jerry Brown; it addressed delays and denials of medical care for injured workers and contained reforms assuring the highest standards for Utilization Review programs. As of July 1, 2018, in addition to requiring utilization reviewing entities to have a Utilization Review program on file with the state, it also required they be URAC accredited if they were to provide modification or denial of treatment requests. With a July 1 deadline, a significant number of the active utilization review entities in California’s workers’ comp system have not obtained URAC accreditation as required under Senate Bill 1160.
CompAlliance’s VP of Patient Advocacy, Glenda Garrard, RN, provides this perspective on the overall impact of this bill and the deadline for URAC accreditation, on the various stakeholders:
“URAC’s main focus is Patient Advocacy, which is most certainly in line with providing the most cost-effective and appropriate medical care. If we assure the injured worker is getting the most appropriate care at the appropriate time, then the injured worker has the best outcome and the employer reduces their expense on unnecessary care.
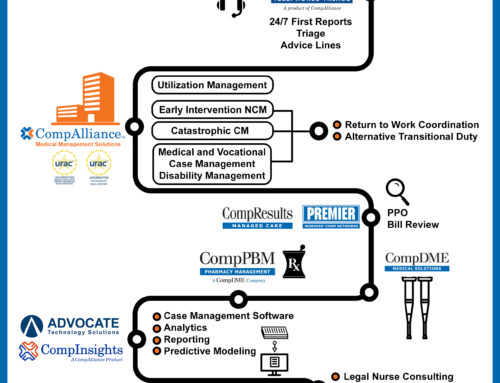
We at CompAlliance believe there is a significant philosophical difference between traditional Utilization Review and our company’s approach, which we refer to as Utilization Management. Our proactive and collaborative approach was developed to assure we take into consideration what treatment the injured worker needs, we expedited that care, and we make sure the care is provided by the appropriate provider.
Today, some vendors are turning Utilization Review into a commodity that boasts of cost savings, but does not track outcomes. Inappropriate denials of care delay outcomes. Therefore, in CompAlliance’s opinion, holding Utilization Review programs to higher standards should benefit employees and employers alike. Since URAC’s standards for UM are focused on outcomes for the injured worker, which in our opinion, should be the foremost driver of the service, we at CompAlliance are fully supportive of the URAC accreditation requirement.”
Among the previously enacted provisions of SB1160 was a 30-day exemption on Utilization Review. For the injured worker, the aim is to reduce treatment delays during the first 30 days following the date of injury. For the treatment provider, many modes of treatment are exempt from utilization review, when the recommended treatment is within the medical treatment utilization schedule (MTUS), including the drug formulary in the first 30 days. If providers show a pattern of deviating from the MTUS, they can lose the exemption, and potentially even be removed from the MPN.
To examine and report on the utilization review process, electronic reporting of UR data is mandated, requiring all Utilization Review data be routed to the Division of Workers’ Compensation (DWC). The new law also prohibits insurers and TPAs from referring UR services to an entity in which they have a fiduciary interest, unless they disclose the name of the entity and their financial interest to the employer and the DWC.
According to the URAC website re: Workers’ Compensation Utilization Accreditation:
“Seeking URAC accreditation for Utilization Review/Management is a method for an organization to demonstrate their commitment to quality, nationally recognized guidelines and evidence-based medicine. You can be assured your reviewer’s processes meet widely recognized national standards and respect both the patient’s and provider’s rights.
URAC is named as a designated accreditor of workers’ compensation utilization review in California, Delaware, District of Columbia, Illinois, Indiana, Maine, Nevada, New York, and Ohio.”
As July 1 approaches, you will need to determine if your UR entity or TPA is URAC accredited prior to this deadline. How can you determine this? You can go onto the URAC Directory of Accredited Companies and search for your current provider.
https://accreditnet2.urac.org/uracportal/Directory/CompanyView/2600