In Part 2 of this series we talked about the The 3 “E’s”, 4 “R’s” and 6 Principles of Trauma Informed Care and their effect on the Trauma-informed Care Process. In this installment we will share how these principles could affect the Case Management Process. As stated previously, they in Part 1, trauma-informed care doesn’t give us more work to do, but rather new tools to do the work we as case managers are already committed to perform. Let’s dig right in.
Trauma-Informed Case Management Process
- Engagement/Initiation of Case Management Services – At the time of case management initiation ask about the meeting environment; ex: door open or closed, avoid forcing eye contact, be aware of your proximity and pay attention to your tone of voice. Explain the rules/expectations of the program and what can the client expect from you? Identify where the client can make choices. Are you engaging in a conversation or asking rapid-fire questions? Are you approaching the person in partnership or as the “expert?” Ask how the RW wants to be addressed.
- Assess – When performing an Initial Assessment ensure confidentiality, offer breaks as needed, develop rapport, avoid asking too many questions initially. Can you work your assessment into a conversation? Explain what you will be asking and why, allow the person to see what you are writing. Develop a shared understanding of the problem. Listen to hear, vs. Listen to fix. Identify strengths and resiliency factors. Assess for past successes. Provide the RW their Rights and Responsibilities during the process of case management.
- Plan – When planning with the RW, use listening skills, prioritize problems, if you say the plan will reflect their goals, make sure it does. Establish goals, action plans and objectives together. What has the RW tried before, what do they think will work?
- Implementation – Ensure ongoing safety while attaining goals, respond to requests for help in a timely manner. Can the RW decide what to work on first? Monitor progress together. One thing I always did as we sat at an appointment waiting to see the physician was to review the RW understanding of their status and what I planned to address with the physician. I always asked if the RW agreed with this plan, did they have anything to add, and would they prefer to bring up these talking points themselves as we met with the physician. The person is the expert on his/her life – reinforce it!
- Evaluation – Ongoing monitoring of progress enables you to respond quickly to a change in the person’s needs. Ask the RW to share their opinion about how things are going. Review goals you mutually agreed upon – are they attained? What has worked, what is not working?
- Case Termination – Explain criteria for termination of services up front. The person, case manager, and other team members prepare for the effects of termination. Identify appropriate referrals. Create an exit plan together. Discuss how to anticipate and resolve future problems. How will the person find additional resources? Do you request feedback from the RW after your services have been terminated?
TRAUMA-INFORMED SERVICES ARE OFTEN ABOUT THE LITTLE THINGS
- Do staff wear clothing that communicates professionalism?
- Does your organization ensure all staff are taught about trauma and its impact?
- Continually assess trauma status
- Value feedback?
- Have a clear plan for dealing with behavioral crises?
- Make every effort to minimize delays
- Speak in a clear, normal tone
- Make eye contact, but be careful not to stare
- Smile, maintain a generally pleasant demeanor
- Be aware of non-verbal communication
- Initiate greetings
- Be open to change, ask for feedback
- Goals should reflect the client’s preferences
- Be sensitive to seating, order of entrance to the physician’s office, who retains any documentation offered by the physician’s office
- Recognize the importance of physical boundaries – any touch including a handshake can trigger a trauma reaction
- Recognize the importance of social boundaries
- Be willing to sit in supportive silence
- Be prepared to repeat information many times
“During every incarceration, every institutionalization, every court-ordered drug treatment program, it was always the same: I was always treated like a hopeless case. All people could see was the way I looked or the way I smelled. It wasn’t until I finally entered a recovery-oriented, trauma-informed treatment program a little more than four years ago, where I felt safe and respected, that I could begin to heal…Someone finally asked me “What happened to you?” instead of “What’s wrong with you?” Tonier Cain
Words have power – Which words could be problematic?
Lazy, Entitled, Piece of work, Frequent Flyer, Liar, Lazy, White Trash, Crazy, criminal, and “Those people”.
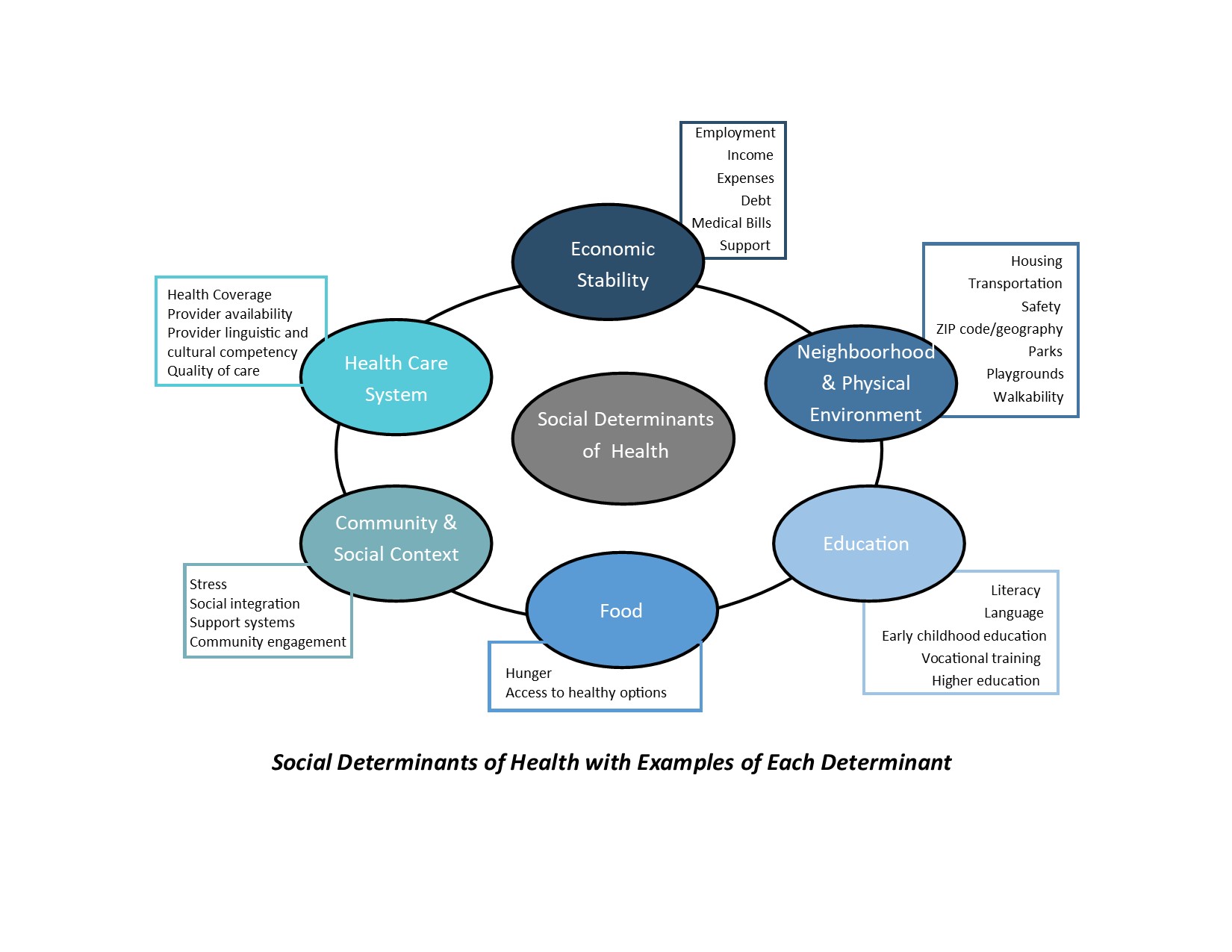
Cultural Competence is important in developing TIC.
Trauma may have different meanings in different cultures and may be expressed differently within different cultural frameworks. It is therefore essential to develop cultural and linguistic competence.
In conclusion, traditionally, we focus on maintaining a healthy and productive workforce centered on job training, technological improvements, and traditional medical care for injury. Instead however the data from the Kaiser Permanente study, Childhood Abuse, Household Dysfunction, and Indicators of Impaired Adult Worker Performance indicates the need to adopt a biopsychosocial approach in which childhood abuse and household dysfunction are understood in terms of their long-term effects on worker health and well-being.