What is Health Literacy?
The Patient Protection and Affordable Care Act of 2010, Title V, defines health literacy as the degree to which an individual has the capacity to obtain, communicate, process, and understand basic health information and services to make appropriate health decisions. Refer to the CDC Health Literacy site for extended information on Health Literacy.
Health Literacy Capacity and Skills
Capacity is the potential a person has to do or accomplish something. Health literacy skills are those people use to realize their potential in health situations. They apply these skills either to make sense of health information and services or provide health information and services to others.
Statistics to Consider
- Nine out of 10 adults struggle to understand and use health information when it is unfamiliar, complex or jargon-filled.
- Limited health literacy costs the healthcare system money and results in higher than necessary morbidity and mortality.
- Health literacy can be improved if we practice clear communication strategies and techniques.
- Clear communication means using familiar concepts, words, numbers and images presented in ways that make sense to the people who need the information.
Two decades of research indicate that today’s health information is presented in a way that is not usable by most Americans. Nearly 9 out of 10 adults have difficulty using the everyday health information that is routinely available. Without clear information people are more likely to not adhere to their treatment plan and can end up in the ER more often. They also have more trouble managing chronic illnesses, such as diabetes and high blood pressure.
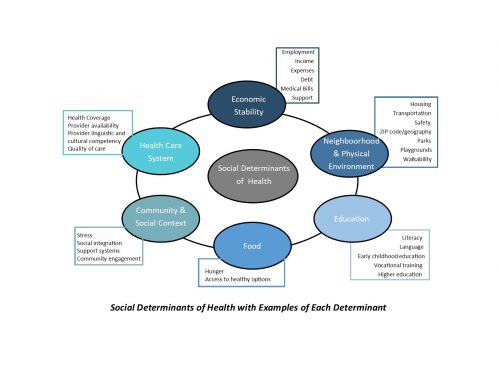
Limited health literacy affects people of all ages, races, incomes and education levels, but the impact disproportionately affects adults over age 65, recent refugees and immigrants, people with less than a high school degree or GED, and lower socioeconomic and minority groups. Limited health literacy is associated with worse health outcomes and higher costs.
Anyone who needs health information and services also needs health literacy skills to
- Find information and services.
- Communicate their needs and preferences and respond to information and services.
- Process the meaning and usefulness of the information and services.
- Understand the choices, consequences and context of the information and services.
- Decide which information and services match their needs and preferences so they can act.
Anyone who provides health information and services to others, such as a doctor, nurse, dentist, pharmacist, or public health worker, also needs health literacy skills to
- Help people find information and services.
- Communicate about health and healthcare.
- Process what people are explicitly and implicitly asking for.
- Understand how to provide useful information and services.
- Decide which information and services work best for different situations and people so they can act.
The responsibility is ours as health professionals to communicate in plain language. Without clear communication, we cannot expect people to adopt healthy behaviors and recommendations. When people receive clear communication, they are better able to act to protect and promote their health and wellness.
Very often there is a deep divide between what the health professional knows and what our consumers (recovering worker) understand. Basic health literacy is fundamental to the success of each interaction between the health care professional and the patient – every prescription, treatment, recovery.
The National Action Plan to Improve Health Literacy seeks to engage all people in a linked, multilevel effort to create a health literate society. The action plan identifies the overarching goals and highest priority strategies that we should pursue to create a health literate society. It is part of a person-centered care process and essential to the delivery of cost-effective, safe and high-quality health services.
Innovative Approaches to Improve Health Literacy
Much of the evidence on intervention comes from simplifying and improving written materials, using video or other approaches to patient education and improving provider-patient communication. Plain language and pictogram information sheets have had many positive results. Strong evidence supports involving members of the target audience in the design and testing of communication products. Because it is impossible to tell who has limited health literacy, one should use a universal precaution approach to health communication – that is assume most patients will have difficulty understanding health information.
Language, culture and identity needs to be considered when communicating health information. Demonstrate an understanding of diverse cultures, languages and perspectives. Incorporate cultural, linguistic and diverse perspectives into health literacy activities and written materials.
CompAlliance’s Approach to Improve Health Literacy
As a URAC accredited case management company CompAlliance decided to incorporate the need for Health Literate communication into our Actions and Communications, both Written and Verbal. We designed two Quality Improvement Projects (QIP) around these goals. (More detail below on the initiatives addressed in each QIP.)
In order to set the stage for these goals and interventions needed to address these goals, CompAlliance performed research as to the barriers to health literacy applicable to our specific case management population.
Barriers to Health Literacy at CompAlliance
- Assumed general lack of health literacy as supported by the research above
- A portion of our workers are non-native English speakers
- Potential lack of understanding of diverse cultures by case management staff
- Potentially not aware of biases (inherent in all people). We all have them
- Communications developed by healthcare professionals – could be too technical for layperson to understand.
After defining the barriers, CompAlliance case management staff brainstormed as to what potential education should be developed for our CM staff, and what potential CM interventions could address the above barriers
- Cultural Diversity Training for all CM staff
- Ethics Training for all CM staff
- Motivational Interviewing Training for all CM staff
- Transitioning of all written worker communications into Plain Language and Linguistically Appropriate translations
- Development of a QIP to follow up with the recovering worker within a specific time frame following the prescribing of a new medication to assess for adherence, side effects, etc.
- Development of a QIP to assess worker adherence to physician treatment plan. This was accomplished through setting up a specific time after each appointment to ensure understanding of the treatment plan and to provide any teaching needed. Timeframes for follow-up with the worker were also specified in between each physician evaluation.
- Patient surveys to be completed at the time of file closure to assess satisfaction with the services provided by case management, including if the case manager provided communications in an easily understood manner.
We in the workers’ compensation industry are all health literacy ambassadors. It is up to you to make sure your colleagues, leadership and community are aware of the issues.