In Part 2 of this series, dated 9/27/2018, I discussed the “What’s in It for the Injured Worker and the Union” regarding RTW. Today I will discuss the common perceptions, misconceptions, the “What’s in it for the Caregiver/Provider” and a best practice statement by the IAIABC. Please refer to my post dated 9/26/2018, for the list of all stakeholders we identified.
Caregivers/Providers
The perception about the provider is that they believe determining when or approving a return to work, is not a part of their job and is not important to the medical healing process.
Reality of why caregivers and providers should care about return to work?
The medical provider may be the first person the injured worker talks to in-depth following their injury. The provider can set return to work expectations right away. In the US, we do not have a specific occupational healthcare system.
Injured workers often see general healthcare practitioners, who may not be very experienced in handling injured workers. Typically, medical providers have little to no training related to return to work. Their primary healthcare provider has potentially established a long-term relationship with the injured worker. Most likely they previously treated the injured worker’s non-occupational conditions. They may now have difficulty in providing objective answers regarding functional capabilities when the injured worker relays reluctance or ambivalence regarding the RTW process.
It is important they understand how much influence they have on injured worker behaviors.
What works?
Throughout care, it is important to objectively evaluate functional improvement and discuss what the injured worker can do both at home and at work. For example, for one of the injured workers with whom I was working, a physician placed a restriction for work of no lifting over 3#. I asked him if the injured worker was unable to lift a gallon of milk at home? The physician clarified, “Oh no, he can lift a gallon of milk at home.” I pointed out a gallon of milk weighs over 8#, so we then were able to put the injured worker’s true capabilities in a more realistic light, for both at home and at work.
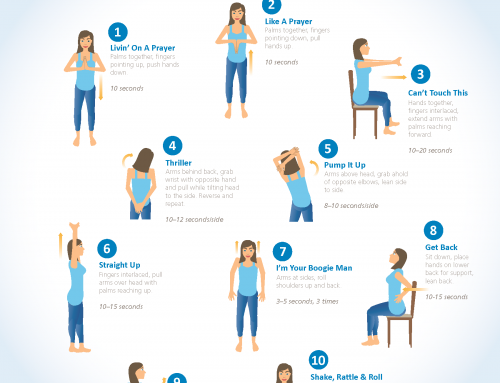
Counseling at every visit helps the patient understand the progress being made and focuses on improvement over impairment. A helpful tool during these discussions is to ask about activities, hobbies, or functions a patient finds rewarding and gear treatment and rehabilitation to achieving these goals also. Aligning functional goals with an individual patient’s wishes will encourage their participation in the recovery process. In addition, providing realistic expectations of results, time frames and what to expect during the recovery process are invaluable.
Encourage patient involvement in his or her own care. One effective strategy is to have the patient keep a journal of the recovery process. A journal helps a caregiver monitor compliance and understanding with a treatment plan. It also allows a patient to see and reflect on progress toward treatment and functional improvement goals. Case managers can be invaluable in this process as at each point of contact we provide objective documentation of status, functional improvement, etc.
The physician should take the initiative to contact the employer, case manager, and claims professional early in the process to understand job requirements and discuss temporary physical abilities and limitation or job restrictions. The physician should provide clear and thorough documentation of the medical facts of the case, provide a written treatment plan, and ongoing functional improvement.
Some jurisdictions are looking toward outcome-based payment models rather than pay for service models. Doctors with good outcomes, like returning workers to the job, will be paid more.
In summary, caregivers should promote early and safe RTW, reinforce the message that RTW is important for both physical and psychological healing, better outcomes should result in higher personal satisfaction and more referrals, RTW should be a key measure of a caregiver’s success in a w/c case. Allowing an IW to stay away from work longer than necessary is not in the best interests of the patient, and caregivers who advocate for RTW help sustain a healthy, safe and vibrant workforce.
The caregiver is one of the first individuals an injured worker interacts with after a workplace injury. What information he or she provides and the way it’s provided creates early perceptions of the quality and benefit of care, the worker’s expectations for functional capabilities, and timely and medically appropriate return to full or modified work. The caregiver’s influence helps determine the worker’s health and return to work outcomes, and all stakeholders’ satisfaction with the care provided.
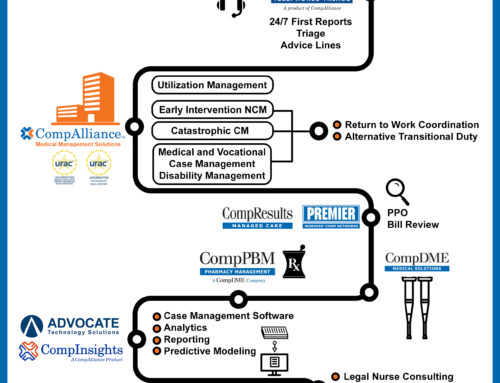
In the next post I will discuss the section of the report that I personally researched, The Role of the Insurer.