I read an interesting article on WorkCompCentral today regarding a class action suit by nurse case managers suing a case management company over the rights to overtime, rest and meal breaks while performing their duties as case managers. The assertion by the case managers was they did not use independent judgment to make decisions; that the decisions were made by physicians and claims adjusters and therefore they were not professionals. Additionally, the plaintiffs asserted nursing, according to California labor Code, specifically excludes registered nurses from the “learned professional” exemption from the overtime law.
I am not from California, and admittedly have never worked in a facility or a state that unionized nurses. My purpose today is not to comment on the result of this lawsuit or whether I agree with the decision that was handed down. Rather when I read this article it made me reflect again on the nursing and case management professions. Are these professions? Are we as case managers professionals? Nurses and other members of the medical profession have wrestled with this issue since Florence Nightingale laid the foundation for professional nursing when she founded her nursing school in 1860.
In 2016 the impetus for revision of the Standards of Practice for Case Management was the need to emphasize the professional nature of the practice and the role of the case manager. There is a disturbing trend in the workers’ compensation and private health industry in which paraprofessionals or claims adjusters are also utilized and referred to as case managers. The laws that limit who can call themselves physicians, nurses, social workers and therapists are what are referred to as “title protection”.
It is not about protecting one’s turf, it is all about protecting the public. The role of the professional case manager utilizes knowledge acquired through advanced education and years of practical experience. It is this knowledge base that empowers the professional case manager to assess not only the illness or injury, but how this illness or injury will impact treatment choices and the consumer’s life going forward (excerpted from Title Protection for Professional Case Managers: What’s in a Name?).
To be clear, case managers are not only nurses. As part of our URAC accreditation in Case Management, we adhere to a clearly defined sets of skills and education required to be a case manager:
“A current, unrestricted license or certification to practice a health or human services discipline in a state or territory of the United States that allows the health professional to independently conduct an assessment as permitted within the scope of practice of the discipline. We must also have a minimum of two years of experience providing direct clinical care to the consumer prior to becoming a case manager.
If the state in which we practice does not require licensure or certification, the individual must also have a baccalaureate or graduate degree (from a nationally recognized educational accreditation organization) in social work, or another health or human services field that promotes the physical, psychosocial, and/or vocational well-being of the persons being served, and must have completed a supervised field experience in case management and must achieve a URAC-recognized certification in case management within four years.”
The official definition of Case Management was updated in 2016 to:
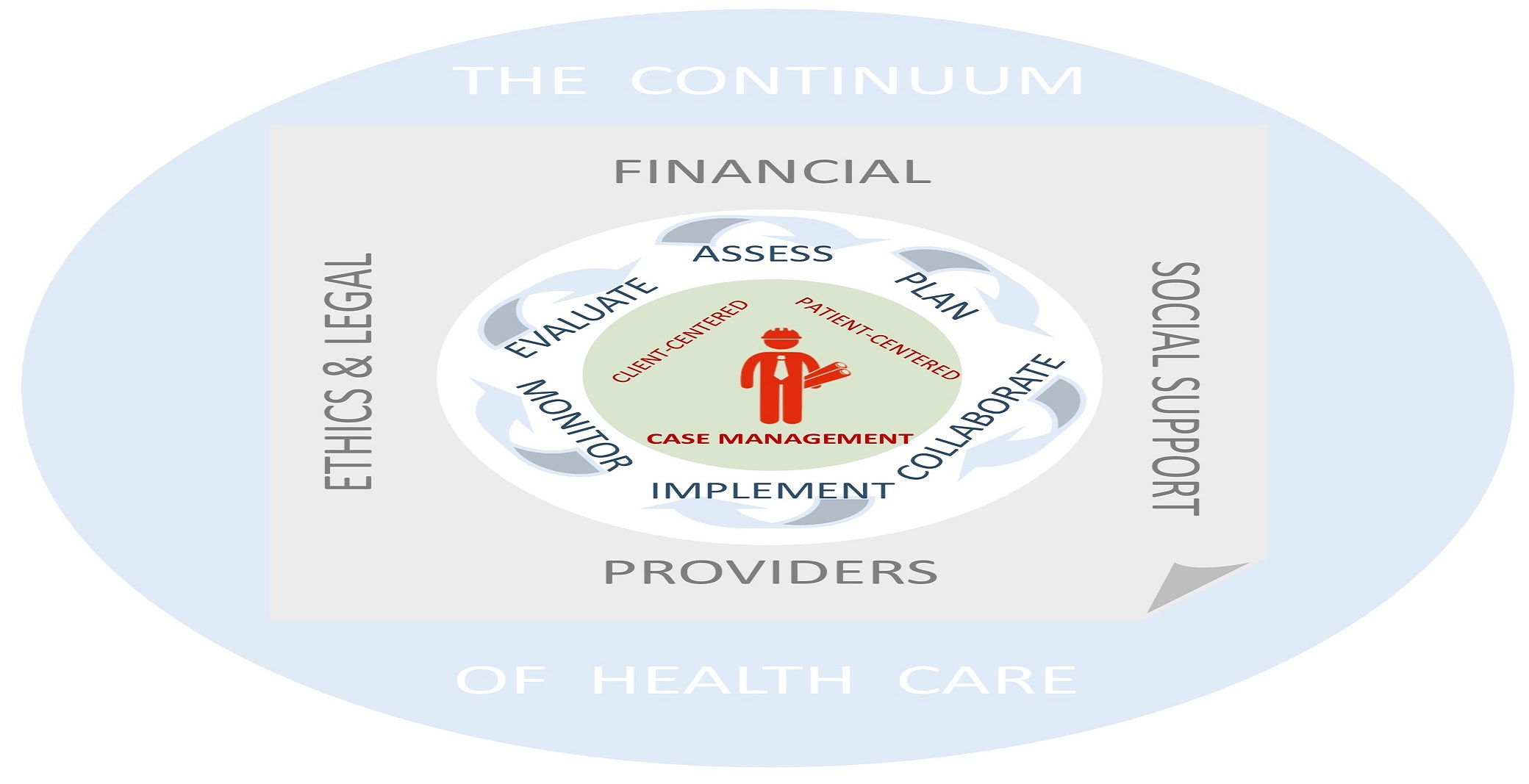
“A collaborative process of assessment, planning, facilitation, care coordination, evaluation and advocacy for options and services to meet an individual’s and family’s comprehensive health needs through communication and available resources to promote patient safety, quality of care, and cost-effective outcomes.”
I also reviewed the CMSA Standards of Practice for Case Management. Throughout the document, case managers are referred to as professionals. Is there a rationale as to why CMSA refers to the case management profession as a profession of professionals? This document states:
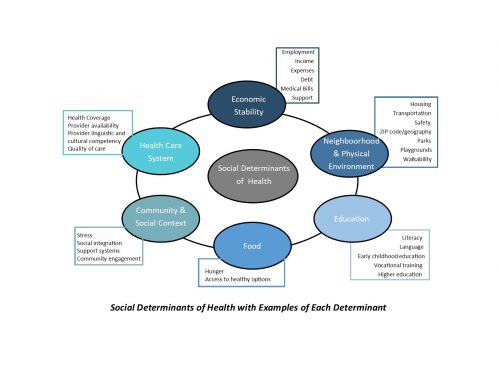
“We recognized the need to revise the Standards of Practice to be reflective of the expanding role of the professional case manager. The awareness that case managers are crucial members of the health care team has been realized providing the need to reexamine and redefine our role in the current complex health care tomography. The body of knowledge required to practice case management is rapidly growing as the specialty continues to evolve. Modern patient care must be based upon the holistic intertwining of information from a variety of disciplines. As our activities become more sophisticated, so must our resources which in turn must remain relevant.
Professional case management is neither linear nor a one-way exercise. Facilitation, coordination and collaboration occur throughout the client’s health care encounter. Collaboration among physicians, nurses, case managers, social workers, pharmacists, allied health professionals, and support staff is critical in achieving the goals of the team, the organization and changing the way we deliver healthcare today. Unity is our strength.”
When I began my practice as a case manager, I was instructed by my supervisor to always wear a suit and carry a briefcase to my appointments with physicians and injured workers. At that time, physicians were not used to a nurse attending an appointment with the injured worker and asking questions about the treatment plan, projections for treatment and return to work, etc. We were told that if you wanted to be viewed as a professional, you were going to have to prove to all parties that you were a professional. You can bet I researched the diagnosis, expected treatment, projections and timelines for treatment, etc. prior to the appointment to prepare for these meetings.
Professional case management evaluates the spending of the all-important health care dollar, while maintaining a primary focus on quality of care, safe transitions and timely access to services. Most importantly it involves ensuring client self-determination and provision of client-centered and culturally relevant care. Case managers are recognized experts and vital participants in the care coordination team who empower people to understand and access quality, safe and efficient health care services while balancing the financial needs of the employer and insurer. In my opinion this is the true definition of the “Triple Aim”.
The case management profession is maturing; it is essential to protect the professional role of the case manager. In addition, the PPACA legitimizes professional case management as an integral and necessary component of the health care delivery system in the US.
Reflecting on all of the above reasons, I stand with the definition of case managers as professionals.