I was reading an ANA Position Statement providing ethical guidance and support to nurses as they fulfill their responsibility to provide optimal care to persons experiencing pain. We in the workers’ compensation industry have participated fully in the national debate on the (in)appropriate use of opioids for pain management. This paper acknowledges the tension between a nurse’s duty to manage pain and the duty to avoid harm.
The American Nurses Association (ANA) believes:
- Nurses have an ethical responsibility to relieve pain and the suffering it causes
- Nurses should provide individualized nursing interventions
- The nursing process should guide the nurse’s actions to improve pain management
- Multimodal and interprofessional approaches are necessary to achieve pain relief
- Pain management modalities should be informed by evidence
- Nurses must advocate for policies to assure access to all effective modalities
- Nurse leadership is necessary for society to appropriately address the opioid epidemic
The nursing profession agrees pain is “whatever the experiencing person says it is, existing whenever he says it does” (McCaffery, as cited in Bernhofer, 2011, para. 2). Nurses and other healthcare professionals have a moral obligation to respond to this patient need (IOM, 2011). Thus, nurses are ethically obligated to act against the disparities associated with access to pain management.
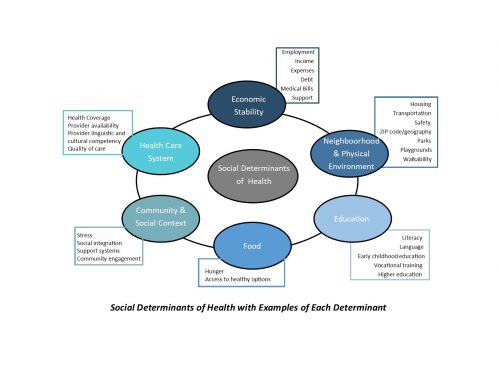
As we have discussed in some of my prior blog articles, effective pain control strategies and all other healthcare decisions, are best made after a complete biopsychosocial assessment and through an informed and shared decision-making model. The plan agreed upon needs to be integrated, multimodal and interdisciplinary in its approach and balances effectiveness with concerns for safety.
Some of the current approaches include pharmacological and a variety of complementary health approaches, such as meditation, acupuncture, dietary supplements, yoga, and exercise. Nurses need to engage in research to identify modalities and strategies to
“(a) prevent, assess, and treat pain; (b) minimize disparities in accessing healthcare; (c) promote societal awareness regarding pain as a public health issue; (d) identify effective educational strategies for nurses, healthcare professionals, and the public; (e) explore cultural meanings of pain; and (f) consequences of undertreating pain.”
There are legitimate reasons to use opioids for acute, post-operative and procedural pain, as well as for patients near the end of life. It is important to understand appropriate non-opioid analgesics/combinations and/or non-pharmacological alternatives that may be equally effective.
As nurses we have an ethical obligation to provide respectful, individualized care to all patients experiencing pain regardless of the person’s personal characteristics, values and beliefs. Have you considered whether you believe an individual of a different age, sex or race should approach their pain differently? One of the methods to address this potential barrier is to examine your personal biases. At CompAlliance we have each of our staff members go through an exercise to examine our biases. We all have them. We must identify our biases and set them aside.
Lack of knowledge about best practices for pain management constrains the nurse’s ability to minimize pain and ensure all avenues for pain management are considered. It is incumbent upon a nurse to maintain competence in their individual practice area. When is the last time you read a peer-reviewed article, or reviewed advances in pain research? Nurses need to incorporate the entire biopsychosocial approach as they do this research.
One of the areas we as a nation are going to need to address is the disparity of providing appropriate pain management treatment. We all know the history by now of the effectiveness of the pharmaceutical industry in emphasizing the pharmacological modalities for pain relief. Effective modalities like cognitive behavioral therapy, or other holistic approaches are many times not approved for reimbursement. When you combine this with the push to decrease the use of opioids, our ability to effectively manage pain can be hampered significantly.
The ANA Code outlines the nurse’s duty to advocate for improved parity in coverage for all effective pain relief modalities. For example, there has been nurse-authored legislation in Minnesota proposing mandatory insurance coverage for acupuncture (Acupuncture service health, 2017).
The ANA Pain Management Nursing: Scope and Standards (2016) concludes all nurses are pain management nurses.
The Position Statement ends with the following summary:
“Nurses have an ethical responsibility to relieve pain and the suffering it causes. The national response to the opioid crisis poses constraints for nurses in every role and practice setting. Recognizing biases, preventing moral disengagement, creating ethical practice environments, and addressing financial inequities are tactics for minimizing constraints and approaching better relief of pain and suffering. In concert with other organizations and associations, nursing will collaborate to provide excellent patient care through research, policy, and education. Guidance from the Code supports these and many other activities to meet the desired ends articulated in this position.”
In Part 2 I will discuss why CompAlliance instituted specific Opioid Protocols and will briefly discuss the concept of NNT and its impact on the CompAlliance pain management protocols in general. Contact US If you would like more information on the CompAlliance Opioid Protocols our Case Management staff utilize.