I just received my CMSA Today magazine (the magazine of the Case Management Society of America) and noticed the magazine this month was focused on the role Case Management plays in a variety of healthcare situations. It made me think about the role we as case managers play in workers’ compensation and what an adjuster should be able to expect from our collaboration on their cases.
There has never been a more challenging time to be a case manager. It is essential that case managers continue their education process. One of the goals for case managers at CompAlliance is for the pursuit of a pertinent case manager certification for both our medical and vocational case managers. One of the main advantages of working with a certified case manager is to maintain their professional certification, the case manager must engage in continuing education pertinent to their certification.
The case manager is a catalyst for change and should facilitate problem solving, education and patient empowerment. I read a recent blogpost by Robert Wilson, “Avoid Attorney Fees by Avoiding the Attorneys” talking about how to avoid attorney involvement on workers’ compensation cases. In my opinion, it all boils down to communication and the timeliness of providing medical care.
Catherine Mullahy writes in an article for CMSA Today, Issue 4, 2017, “Success Requires Mastering Today’s Challenges”
“Advocate for your true role as a case manager. Recognize that, while utilization review has a role to play in the efficient use of resources, and appropriate reimbursement for services provided, it is case management that truly achieves improved outcomes, the engagement of patients as partners in their care, avoidance of readmission and improved transitions of care. Additionally, case management is critical to improved patient satisfaction rates, which have become increasingly more important.”
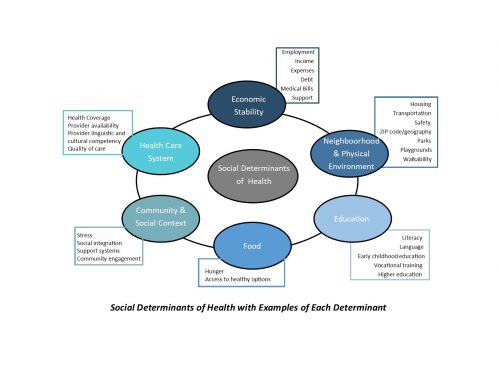
Using a case manager on your complex claims be they due to complex trauma or co-morbidities impacting the healing process, can help in a variety of ways. The case manager will begin with obtaining a comprehensive medical, prescription, social and work history. This will assist with defining co-morbidities of which you may not even be aware. For example, determining if there are prior medical or psycho-social conditions that may impact case progression, clarification if the injured worker was on an opioid prior to this current injury, and assist with setting initial reserves. This initial history taking also serves to establish a communication channel and rapport to hopefully minimize the need for attorney involvement on the case.
The case manager will work with the employer, when approved to do so, to obtain a current Job Description, ascertain if light duty is available, and facilitate progression of duties during the rehabilitation process. The case manager can assist with keeping the employer and injured worker connected, and exploring alternatives for light duty. WCRI studies detailing the Major Predictors of Worker Outcomes in Wisconsin,
“Concerns about being fired were associated with a four week increase in the duration of disability, 20% reported significant problems getting services they or the provider wanted, (double the rate of workers not concerned about being fired), and 18% reported dissatisfaction with care, (vs. 8% of workers not concerned about being fired).”
The case manager reports back after each appointment with information as it relates to the job of injury to the employer. The case manager keeps the adjuster informed not only of the treatment recommendations and projections made by the physician, but also if these meet evidence-based guidelines for treatment and RTW projections. If treatment or RTW projections are outside of evidence-based guidelines the case manager can assist with coordinating an IME or Utilization Review.
If the Injured Worker is prescribed opioids, the case manager can work with both the treating physician and injured worker to explore alternatives and minimize or eliminate ongoing prescribing. Education regarding safe storage, utilization, disposal, etc. is paramount. If the Injured worker has been on opioids prior to referral to case management, the updated CDC Guidelines for Prescribing Opioids can be reviewed with the physician and injured worker and alternatives for the weaning process can be explored.
As an adjuster, you can expect the case manager collaborating with you on your complex files to work to engage the injured worker in their care, to work towards patient adherence to their agreed upon treatment plan, effective communication with the employer, facilitation of a timely and medically appropriate return to work, minimize or eliminate opioid prescribing, and communication of the treatment plan and analysis if this treatment meets evidence based guidelines. Keeping these communication channels open should further assist in minimizing injured worker dissatisfaction and the perceived need to engage the services of an attorney.