Why is medication reconciliation so important when controlled prescription drugs are prescribed?
In my last post I discussed some of the best practices a case manager should be utilizing when opioids or other controlled prescription drugs are prescribed for the injured worker. One of those tools described was Medication Reconciliation. Medication reconciliation is a formal process for creating the most complete and accurate list possible of a patient’s current medications and comparing the list to those in the patient record or medication orders.
According to the Joint Commission, Medication reconciliation is the process of comparing a patient’s medication orders to all of the medications that the patient has been taking. This reconciliation is done to avoid medication errors such as omissions, duplications, dosing errors, or drug interactions. It should be done at every transition of care in which new medications are ordered or existing orders are rewritten. Transitions in care include changes in setting, service, practitioner, or level of care. This process comprises five steps: (1) develop a list of current medications; (2) develop a list of medications to be prescribed; (3) compare the medications on the two lists; (4) make clinical decisions based on the comparison; and (5) communicate the new list to appropriate caregivers and to the patient.
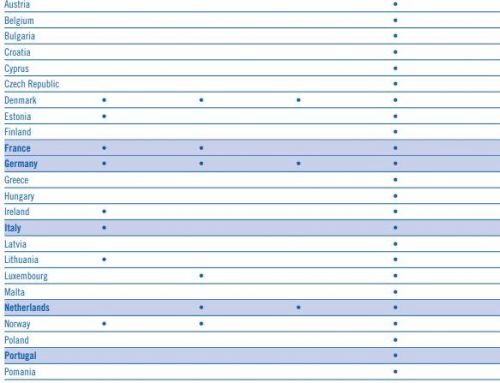
Why is this so important in workers’ compensation? The Joint Commission added medication reconciliation across the care continuum as a National Patient Safety Goal in 2005. The Institute for Healthcare Improvement (IHI) has medication reconciliation as part of its 100,000 Lives Campaign. In the workers’ compensation setting obtaining a complete listing of all medications, vitamins, dietary supplements, etc. at the initiation of a case serves many purposes. It will alert all healthcare providers as to potential co-morbidities, and ensure treatment is adjusted if needed. (This is a topic for another day.)
A complete listing of all medications can assist in preventing drug interactions. It can also serve as an opportunity for the case manager to assess the injured worker’s understanding of their medications, how to take them, and to ascertain if education is needed.
Additionally, if the injured worker utilized controlled prescription drugs prior to the reported injury – opioids, muscle relaxers or any anti-anxiety medications, this needs to be documented and taken into account as treatment progresses and any medications are considered. The best time and most likely most accurate history to be obtained, is at the onset of the case.
The best results for medication reconciliation are obtained when the following items are specified: a consistent format for obtaining this history is utilized, a time for obtaining and updating this history is specified in case management procedures and also how to communicate this information to the appropriate stakeholders.
The ultimate goal for medication reconciliation is to prevent medication errors and to prevent the adverse effects of drug events. A side benefit of medication reconciliation is an opening of dialogue between the injured worker and the case manager, assessing needs for education and also identifying prior usage of controlled prescription drugs.