In 1987, Health Minister Michèle Barzach imposed the liberalization of syringe sales in France. For a long time, the struggle against HIV rested on this political measure alone. In Europe, buprenorphine for the treatment of opiate addiction was first registered in France and by the year 2000 was available in eight Member States of the EU. However, its availability to most potential patients in the EU continued to be limited in comparison with methadone treatment. In contrast, in France, buprenorphine treatment for opiate dependence has spread out quite rapidly since the mid-1990s.
It was estimated in 2003 that 77% (83,000 of 107,000) of the buprenorphine treated patients in Europe were in France. Another important change in France, in contrast to other European countries, is that most buprenorphine-treated patients receive their buprenorphine prescriptions from general practitioners (GPs) in primary care or office-based settings, with dispensing in community-based pharmacies happening in a relaxed regulatory context.
This policy has had a direct, positive impact on the number of deaths caused by heroin overdose, which was reduced by four-fifths between 1994 and 2002. In 2014, there were 370 reported overdose deaths in France contrasted with a population of 66.13 million. In 2017, in the US there were 70,237 drug overdose deaths contrasted with a population of 325.7 million. Additionally, in France in 2016, there were 49 HIV diagnoses attributed to injecting. In the US, in 2017, the number of HIV cases attributed to injecting was 2,648.
Drs. Fatseas and Auriacombe write in a paper analyzing why buprenorphine for treatment of opiate addiction is so popular in France, that the French approach has potential advantages and drawbacks.
“On one hand, making treatment easier to access could increase the number of individuals in treatment; on the other hand, a lack of regulation could increase the occurrence of buprenorphine side effects or diversion to clinically inappropriate patients and thus limit the overall benefit of this medication.”
The physicians that prescribe buprenorphine are more often in a health care network and have received some additional treatment in drug maintenance, though this is not a requirement for prescribing buprenorphine.
Some of the rationale for increased buprenorphine prescribing in France according to Drs. Fatseas and Auriacombe:
- The pharmacologic profile of buprenorphine – similar in benefits to methadone in treating opioid dependence, it is long-acting like methadone, but not due to a long plasma half-life, but rather its high affinity for the μ receptor. It is a partial agonist at the μ receptor, making overdose unlikely. Drug cessation is associated with milder levels of withdrawal distress, and there are more flexible dispensing options.
- Methadone and buprenorphine prescribing regulations in France – Only physicians working in state-licensed substance abuse clinics or hospitals can initiate a methadone prescription that is initially dispensed only on site. Urine testing is compulsory. Once the initial prescriber has determined that the patient is stabilized, clinical management of the patient and methadone prescription may be transferred to any medical doctor. At that point, dispensing may be done from any pharmacy in the same manner as for buprenorphine. As described above, GPs may prescribe buprenorphine, and any pharmacy may dispense. No specific training is required. The maximum duration of a buprenorphine prescription is 28 days, and the maximum number of take-home doses is seven. However, a physician can override this rule either by requesting that the pharmacist provide daily, supervised dosing of buprenorphine or dispense up to 28 days of take-home doses. There is no regulatory requirement for urine testing.
- Characteristics of the French health organization – The French health care system is based on a pay-per-service basis with universal medical coverage. The Social Security system acts as a universal medical insurance that covers more than 90% of the population, regardless of their economic situation, legal status, or nationality. This facilitates the treatment of marginalized individuals. A GP is paid 21 euros for an office visit, regardless of duration or frequency. Ordinary consultations are reimbursed at a 65% replacement level.
However, if the patient has a chronic illness, reimbursement covers 100%, and the payment can be made directly from Social Security to the GP. Because opiate dependence qualifies as a chronic illness in the French health care system, payment is fully covered by Social Security. In addition, there is a dense psychosocial support service funded by local authorities at no charge to those in need. Further, patients with opiate dependence can be treated in special substance abuse treatment centers supported by Social Security funds.
French pharmacies provide a range of clinical services. For example, the medication itself can be dispensed and taken at the pharmacy under the pharmacist’s supervision daily, if required. In this context, pharmacists play a crucial role in the dispensing of treatment, in monitoring clinical improvement of subjects, and in informing the prescriber about any difficulties. Overall, the French health care system supports a substantial amount of care within primary care settings through medical and social support and through the possibility of supervised dispensing through pharmacy services
This office-based primary care model increased the number of heroin problem users accessing treatment, far exceeding treatment access to methadone programs in specialist centers. This impact was parallel to low-cost actions. Currently, treatment dispensed in French primary care settings appears to be a cost-effective strategy for treating opiate-dependent subjects compared with specialized centers.
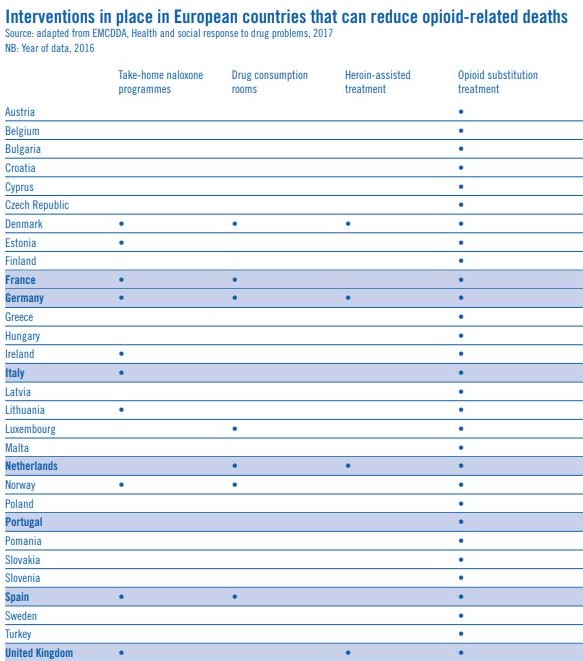
In 2016, France opened its first consumptions rooms in Paris and Strasbourg as part of a six-year pilot experiment. French public health workers would like to open more rooms, but they aren’t exactly embraced yet. Visitors must be 18 years or older and declare whether they are drug injectors or drug smokers. Inside there are 12 injection and four smoking spots. During their first visit they must give some type of ID in order to track the number of visitors. They must sign an agreement saying they are not allowed to share, sell or buy inside the consumption room.
Rapid testing is available for both HIV and hepatitis C. Consumption room staff store hepatitis C medication for those who live on the street, so it is not lost or stolen. After checking in, visitors must wash their hands and get new syringes and supplies. They have 20 minutes to inject and they move to the “chill out” room, a stylish, comfy space with bean bag chairs, books and plants. They can hang out as long as they want, and there is no limit to the number of times someone can visit in a day. Medical staff is nearby in case of OD. There have been only three centers started in Paris in two years, due to local resistance to the centers.
To address addiction, the French look beyond drugs to caring for the person. There are more than 300 harm reduction centers and 480 clinics that offer opioid substitution treatment and other medical treatment anonymously and free of charge. The services include safe places to sleep, checking street drugs for unwanted substances and reaching into the countryside to help rural users, through mailing injection kits, with a variety of items that can be ordered to include male and female condoms, doses of lubricants, flyers and brochures on Hepatitis C, AIDS and harm reduction. The majority of those who order the kits live in towns with fewer than 5,000 inhabitants.
Positive effects of substitution – Substitution has had three positive consequences, according to the authors of the SWAP report, June 2018. First, widespread prescription of substitution medication made it possible to treat and prevent viral infections. The number of HIV infections collapsed among people who inject drugs (PWID). Second, substitution treatment led to a major decrease in the incidence of overdose. Third, substitution partially updated a once-chaotic course of treatment for people who are dependent on heroin. We have also observed a lower incarceration rate and a decrease in petty crime associated with opioid trafficking.
Negative consequences of substitution – It is noted approximately 15 – 40% of patients inject their high-dose buprenorphine, and in these cases, it is recommended providers prescribe syrup-form methadone instead, which is much harder to inject. High-dose buprenorphine trafficking has also emerged, especially in three regions of greater Paris. From the description of the process by which this diversion happens, there does not appear to be a Prescription Drug Monitoring program in place, such as in the US, to prevent from unscrupulous overprescribing or inattentive dispensing.
Items to consider from the French model include as I have advocated for in the past – in the US we need to encourage MAT at the primary care level to increase access to treatment. Also, how will we reimburse for the time it takes to provide this more complex level of treatment? How do we provide this treatment to uninsured patients? How do we remove the stigma?