Objectifying that “Gut Feeling” when controlled prescription medications are prescribed for acute or chronic pain
In a previous post we discussed the need to set up protocols based on best practices when case managing an injured worker prescribed a controlled prescription drug. One of the elements to consider is utilizing standardized assessment tools to objectify that “gut feeling” your injured worker is not appropriate for opioid therapy.
ACOEM guidelines sanction opioid therapy for acute pain only when there is significant objective evidence of injury or when other drugs are contraindicated and for short term used in chronic pain to facilitate physical activity. This type of use should be infrequent and other therapy options should first be exhausted.
Consider the following scenario: A 53 year old female injured worker who has reported a low back injury and the case manager is meeting with her for the first time at her physician’s office. Ms. Smith retained an attorney who has instructed her not to sign or complete any paperwork provided by the case manager.
During the initial assessment meeting with the case manager Ms. Smith provides a verbal consent to participate in the case management process and is cooperative with providing her medical and social history and does participate in the medication reconciliation process.
Ms. Smith has been treating for the past 6 weeks with an orthopedic surgeon and has been prescribed an opioid pain medication (which she reports she ran out of three days ago and is now in a much higher level of pain), a non-steroidal anti-inflammatory and reports she has not achieved any relief of her initial pain with medications and physical therapy.
Ms. Smith is not able to describe to the case manager her home exercise program without looking at her sheet from the physical therapist and relates she is frequently in too much pain to do her home program. Her physician has kept her off work during this initial six weeks.
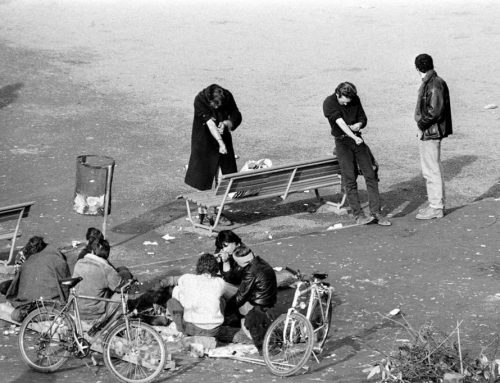
Her MRI shows mild disc bulging, she smokes 2 packs per day and is 30# overweight. She states she has a history of depression and takes an anti-anxiety medication prescribed by her personal physician. When reviewing her PT attendance, the case manager notes Ms. Smith missed 2 sessions and was late for 3 sessions. She stated she missed and was late for her therapy sessions because she was having trouble finding daycare for her 2 preschool grandchildren that live with her.
Based on the above scenario, many red flags are noted. First and foremost, Ms. Smith has been prescribed an opioid for 6 weeks with no reports of reduced pain or improvement in her functional capabilities. She remains off work. She used up her current opioid prescription prior to her scheduled appointment. It is anticipated the physician may continue prescribing opioids at this upcoming appointment.
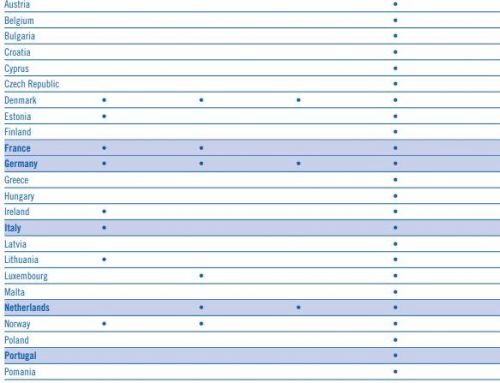
Beyond taking a good medical history via effective patient interview, there are several risk assessment tools that may be used to further evaluate how likely it is that patients will have difficulty using opioid analgesics as prescribed. The choice of the tool depends on the time available, format of the assessment, etc. The assessment tool CompAlliance has elected to utilize [DIRE] is a nationally standardized tool that can be completed by the case manager based on the results of the Initial Assessment conducted with the injured worker.
The results of this assessment can then be discussed with the prescribing physician and assist in opening a dialogue to discuss alternatives to treatment. This assessment will also assist the case manager in developing goals in collaboration with the injured worker for increasing adherence, participation and “buy-in” into their rehabilitation plan.