PDMP & Evidence Based Guidelines – Designing Opioid Protocols for Case Management
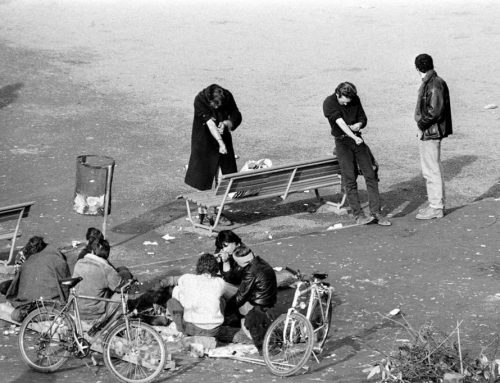
What is a PDMP? Prescription Drug Monitoring Programs collect, monitor, and analyze electronically transmitted prescribing and dispensing data submitted by pharmacies and dispensing practitioners. The data is used to support states’ efforts in education, research, enforcement and abuse prevention. PDMPs are managed under the auspices of a state, district, commonwealth, or territory of the United States. Prescription data is provided only to entities authorized by state law to access the program, such as health care practitioners, pharmacists, regulatory boards and law enforcement agencies.
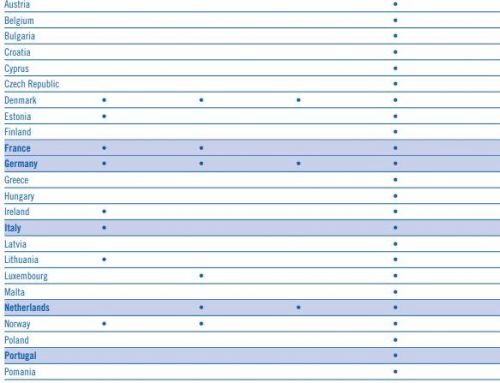
Currently, 49 states, the District of Columbia and one U.S. territory (Guam) have legislation authorizing the creation and operation of a PDMP [Missouri is the only state exception.] The State Profiles have a link to each state’s laws and rules governing their PDMPs on the PDMPTTAC website.
PDMPs are simple in concept but complex in execution, according to Dr. Lynn Webster in his article that describes their potential and shortfalls. How does the case manager facilitate usage of this data? As the PDMPs have been enacted in each state in which we practice, CompAlliance has been documenting in our introductory letters to the prescribing physician a request to access the PDMP applicable to their state when a controlled prescription drug (CPD) is prescribed. The case manager requests the physician access the PDMP each time an additional dose of a CPD is prescribed. This results of these inquiries are relayed to the claims professional on an ongoing basis.
The case manager should also be aware of sources such as the MDA, ACOEM, Cochrane Collaboration and ODG which provide comprehensive and up-to-date research regarding medical treatment and return to work guidelines for a specific diagnosis. These evidence-based decision support tools assist in providing benchmark outcomes in workers’ comp, non-occupational disability and general health insurance.
Evidence based medicine is not a cookie cutter approach and the Initial Evaluation and Medication Reconciliation (described in Part 2 of this series of articles) performed by the case manager at the inception of the case also assists in identifying any co-morbidities that may impact the treatment plan, medications prescribed, rehabilitation plan and RTW.
These support tools assist the case manager in her collaborative efforts when working with the treating physician. They serve as the basis for requesting the documentation needed to clarify medication or treatment plans that do not fall within evidence based guidelines.